A long COVID classification approved by the World Health Organization is developed at St Petersburg University
St Petersburg University scientists have set up the interim results of the work of the Centre for the study of long COVID over the past 12 months. The doctors spoke about: the first reference to the so-called long COVID in the world; which symptoms are most common in such patients; and how deep sleep can help overcome the effects of COVID-19.
The first mentions of long COVID appeared on social networks in the spring of 2020, a few months after the pandemic broke out. When describing their condition after the recent illness, people used to refer to it as a "long COVID". At the same time, British epidemiologist Paul Garner was the first to identify the problem in the scientific literature. He called his experience of living with COVID-19 a "roller coaster of ill health".
The discussion took place within the framework of the 10th St Petersburg International Health Forum, at the conference titled "Organisation of Admission of Patients with Post-Viral Manifestations Illustrated by Long COVID".
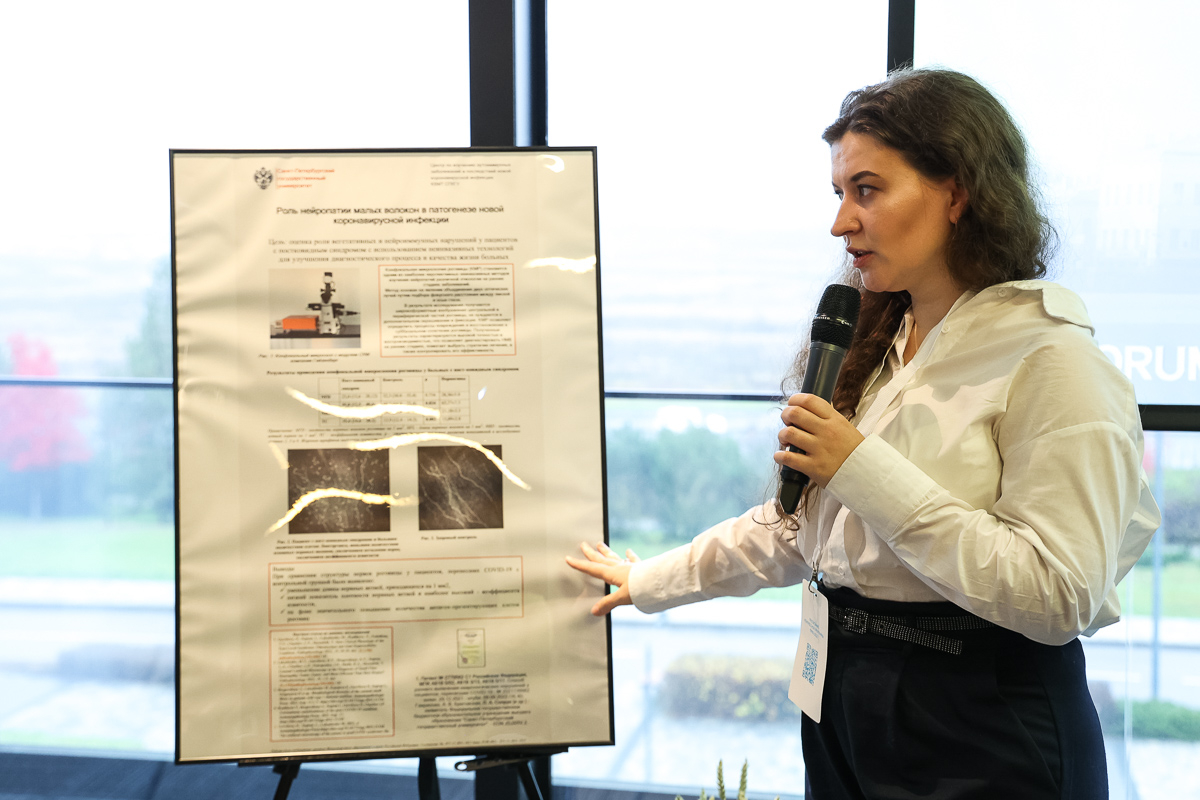
In autumn 2021, the Centre for the Study of Autoimmune Diseases and the Effects of the New Coronavirus Disease named after Professor Yehuda Shoenfeld was opened at St Petersburg University. That was the first place in the world gathering a team of experts who combined real work with patients, the development of treatment guidelines and scientific work in the field of studying the new virus.
The employees of the centre reported that, during the 12 months of their work, 524 patients had visited them. All of them had gone through COVID-19 and felt uncharacteristic symptoms after that. Usually, their discomfort developed not immediately after the illness but three or four months later. Most often, patients complained of: shortness of breath; "fog in the head" i.e. impaired attention; rapid heart rate; loss of smell; impaired hearing, vision and sleep; prolonged fatigue; anxiety; tingling in the limbs; fever; and pain in the joints − a "flu-like syndrome". At the same time, surprisingly, experts notice that long COVID occurred after a mild or moderate disease more often than after a severe one.
Scientists note that, to diagnose a patient with a long COVID, the doctor has to rule out any other pathologies, and the patient’s symptoms must persist for over two months.
Usually, patients come to us with thick batches of documents, their clinical records. They visit a cardiologist with tachycardia and a rheumatologist with a pain in the joints. Yet it turns out to be impossible to accurately diagnose a patient without studying long COVID as such. Complex studies and work of a team of doctors are required.
Lidiia Soprun, an epidemiologist, expert in the Centre for the study of long COVID
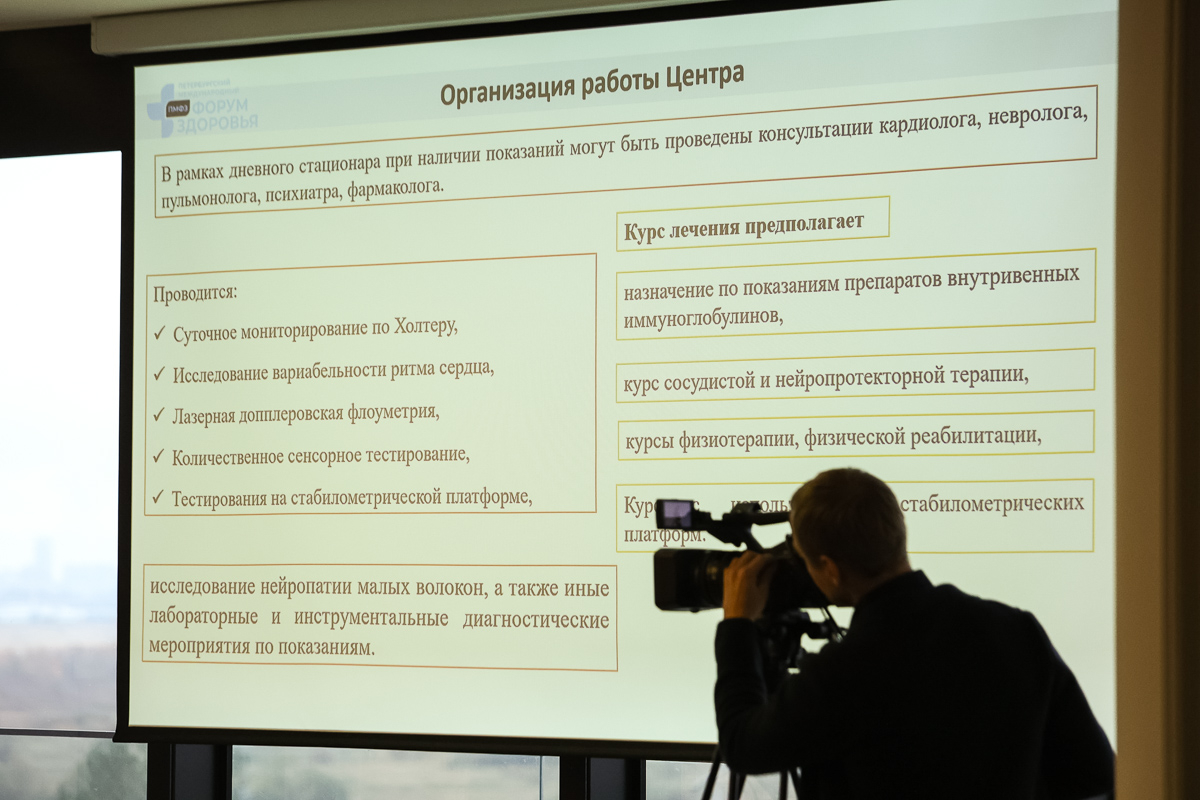
At the St Petersburg University Clinic, the patient undergoes an initial consultation, with their problem being studied comprehensively. ’At our day patient department, patients are treated by cardiologists, neurologists, pulmonologists and psychiatrists,’ said Pavel Kislyi, Head of Day Patient Department № 1.
Thus, by studying a variety of cases, the doctors of St Petersburg University developed a new classification of long COVID that was approved by the World Health Organization. The classifier is based on the division of patients according to their phenotypes. For example, scientists have identified the fibromyalgia type. In this case, the patient suffers pain in the places of muscle attachment. An increased muscle tone and spasms are also observed. Another phenotype is a pulmonological one. It is one of the most common phenotypes. It is characterised by constant shortness of breath, burning pain between the shoulder blades or behind the sternum in the absence of significant changes on the X-ray and CT scan of the chest and in the study of the cardiovascular system. The scientists identified a total of six phenotypes.
COVID-19 is included in the list of diseases dangerous to public health, along with HIV, hepatitis B and C, anthrax, smallpox, cholera and some other diseases.
Based on the data obtained, the scientists developed treatment guidelines for patients diagnosed with long COVID. It is noteworthy that, in addition to drug therapy, doctors also use non-drug methods. Thus, the observance of sleep hygiene is very effective and useful for patients. It is important to adjust the environmental factors to your regime. That includes reducing the sound with the help of earplugs, and achieving complete darkness, which increases the duration of the deep sleep phase, with the help of sleep masks and thick curtains. Experts drew attention to the fact that, without healthy sleep, drug methods will not be able to work effectively, since the body needs time and effort to recover. These processes take place best of all when you are asleep.
For regions with a cold climate and a shortage of sunny days, doctors advise light therapy methods, i.e. treatment with artificial light sources. The recommendations also include: following a diet, such as a gluten-free one helping to relieve inflammation in the gastrointestinal tract; maintaining a fluid-and-electrolyte balance; and physical activity.
Patients from all over Russia come to the Centre for the Study of Autoimmune Diseases and the Effects of the New Coronavirus Disease at St Petersburg University. They pay for the initial consultation themselves, and after a long COVID diagnosis is made, treatment is carried out at the expense of the federal budget allocated by the Compulsory Medical Insurance Fund.