St Petersburg scientists assess the dynamics of immune response to COVID19 in St Petersburg
Researchers from St Petersburg University and the Molecular Biophysics Division at B.P. Konstantinov Petersburg Nuclear Physics Institute have quantitatively characterised the dynamics of the immune response in a group of volunteers from St Petersburg. The result is that the immunoglobulins of IgA class play a key role to achieve a herd immunity. These immunoglobulins remain in the blood of those who have suffered from the coronavirus, sometimes even after eight to nine months, i.e. much longer than when reacting to other viruses.
The research findings are published in the Journal of Medical Virology, that is a peer-reviewed journal in medicine .
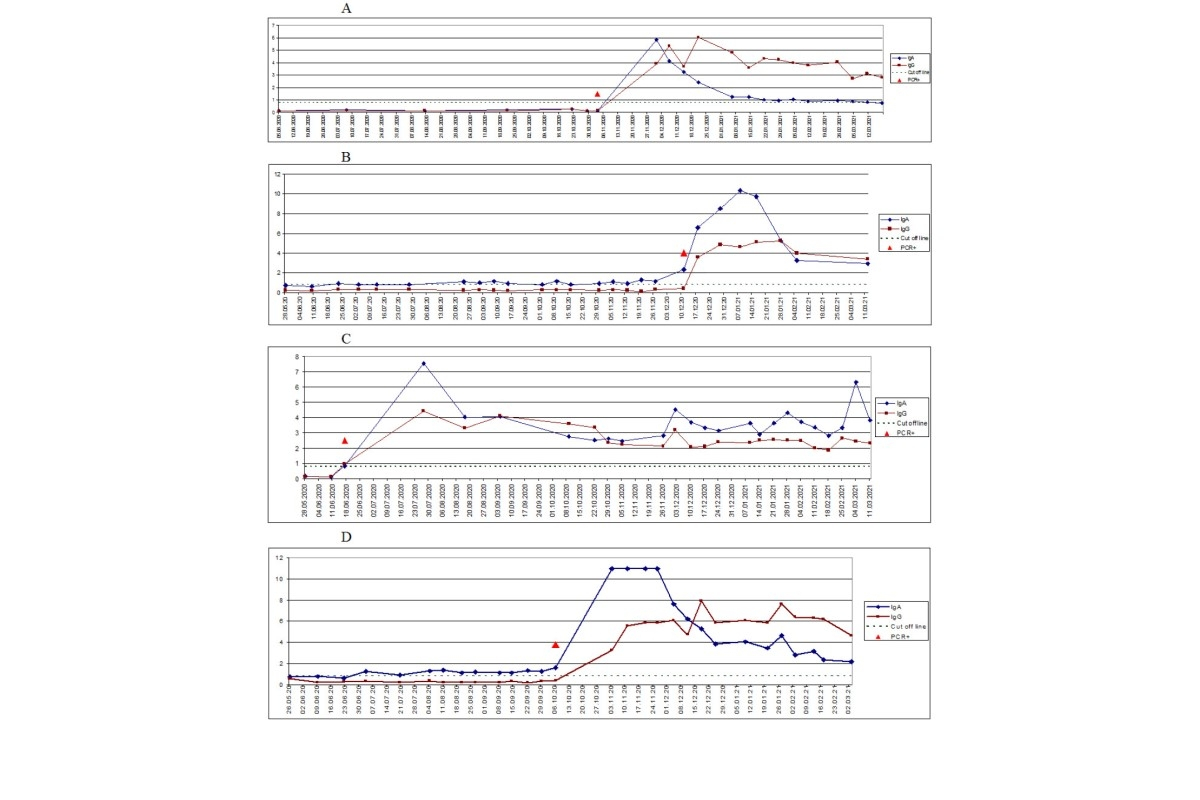
Over a year ago, scientists started a biomedical study that focused on how to achieve a herd immunity to COVID-19. It tracked the dynamics of how IgA and IgG antibodies occurred and changed in 180 volunteers during the epidemic. Each 10 to 14 days from May 2020, those who participated in the study donated biomaterials to determine the level of immunoglobulins. Some of them fell ill during the 'first wave' (May-June 2020); most of the cases appear during the 'second wave' (October-December 2020); and majority of those who took part in the study did not have the coronavirus detected.
Antibodies are protective protein complexes produced by the immune system in response to an infection in the body. Class A immunoglobulins (IgA antibodies) are among the first to be produced during the active phase of the disease and dominate the body secretions (saliva, mucous secretions, digestive juice). Immunoglobulins IgG are found in blood plasma and usually begin to be produced about 10 to 14 days after the onset of the infectious process. Their presence indicates that the long-term immunity is achieved. They destroy cells of pathogenic microorganisms and virus particles.
Andrei Ivanov is Head of the Department of Human Genetics at the Pirogov Clinic of High Medical Technologies at St Petersburg University and the author of the study.
According to him, how the body can be protected can be divided into three phases or stages, each of them having its own specifics.
The first stage is innate immunity. It is an evolutionarily ancient and therefore strong defence system that releases molecular agents into the human body. This forms an early inflammatory response.
The second stage is cellular immunity. Cells are engaged in constant interaction and form a complex defence system in our body. This system is as complex as the nervous system. Finally, the third is humoral immunity. Its main weapon is antibodies, i.e. molecular complexes that recognise antigens and help the body fight a virus or an inflammation.
All these stages are firmly interconnected. It is almost impossible to imagine how they can work separately. In modern diagnostics, how the disease progresses and how the body responses to the disease are assessed by measuring the level of antibodies in the blood and by quantitatively assessing the effect of cellular immunity. These are the indicators that the scientists studied in relation to how the herd immunity to COVID-19 was achieved.
'Most viral infectious diseases in humans are associated with a rapid increase in IgA and then IgG. After three to four months, the level of IgA decreases and reaches the values that are not recorded in the tests, while the level of IgG reaches a peak in one and a half to two months and then it gradually decreases,' said Andrei Ivanov.
Yet how our immune system responses to the Sars-CoV-2 coronavirus is different. In most of the participants who had suffered from the disease, the IgA level remained high even eight to nine months after recovery and significantly exceeded the level of IgG in the blood.
Andrei Ivanov, the author of the study and Head of the Department of Human Genetics at the Pirogov Clinic of High Medical Technologies at St Petersburg University
The project involved 180 volunteers, with 51 people (28%) falling ill during the observation period. Everyone who underwent COVID-19 developed a stable immune response, yet the individual immune status was specific in each case. In about 39% of patients (20 out of 51), high IgA levels persisted for more than six months. In a third of patients with COVID-19 (17 out of 51), the IgA level was higher than the IgG level. At the same time, approximately 15% of those who took part in the study (28 people out of 180) had an increased level of IgA from the start of the study and it remained the same throughout the observation period.
'This means that IgA can be found in people without coronavirus and shows a stronger and more robust response to the SARS-CoV-2 virus than IgG. In this case, we should distinguish between plasma and secretory IgA. Secretory IgA are secreted on the mucous membranes of the upper respiratory tract. This is one of the first barriers where the coronavirus can enter into the body. They can neutralise the virus and prevent the binding of virus particles with the surface receptors and subsequent infection of a healthy cell. In our study, we analysed plasma antibodies that were found in blood plasma. In most people living in the pandemic, how our body fight SARS-CoV-2 is associated with this element of the body's antiviral defence system,' explained Andrei Ivanov.
However, the presence of IgA in the blood does not necessarily indicate that our body can resist the disease. One participant with an increased level of the antibodies in the blood fell ill with COVID-19.
The results of the study show that there is an individual immune response to the disease, which is not however related to age or gender. The probability of getting sick is practically the same whatever your age or sex is.
All of those who took part in the study had an active social lifestyle and how likely they were to be exposed to coronavirus was almost the same as for most people in St Petersburg.
In the study, there were no cases of a severe disease that would require hospitalisation, i.e. all those infected had asymptomatic COVID infection or it was in a mild form.
The monitoring carried out allows for the first time to track the dynamics of the immune response and draw conclusions about how the herd immunity can be achieved, said Andrei Ivanov.
When infected with the coronavirus, our body is undergoing a large-scale 'malfunction' in the immune system. This may trigger autoimmune processes and lead to a cytokine storm. Measuring IgA can help detect these changes and initiate timely therapy.
Andrei Ivanov, the author of the study and Head of the Department of Human Genetics at the Pirogov Clinic of High Medical Technologies at St Petersburg University
A decrease in IgA levels shows the need for vaccination and protection of the body after suffering from the coronavirus, which is essential for people with autoimmune diseases and weakened immunity, as the scientists concluded. Analysis of the level of antibodies in the blood of patients, according to the researchers, can help in calculating the time of vaccination and revaccination after the infection. This is essential in planning the vaccination campaigns and assessing whether the herd immunity has been achieved.
Learn more about how to get vaccinated at St Petersburg University.

