N + 1: "Trace amines are very tasty". Raul Gainetdinov about the most understudied class of biogenic amines and the basics of aromatherapy
It is quite difficult to make real scientific breakthroughs nowadays. To discover something fundamentally new in a highly competitive environment is an almost impossible task. This is especially true for research areas where most of the fundamental discoveries have already won all the highest scientific awards. In contrast, the under-researched topics are considered unpromising.
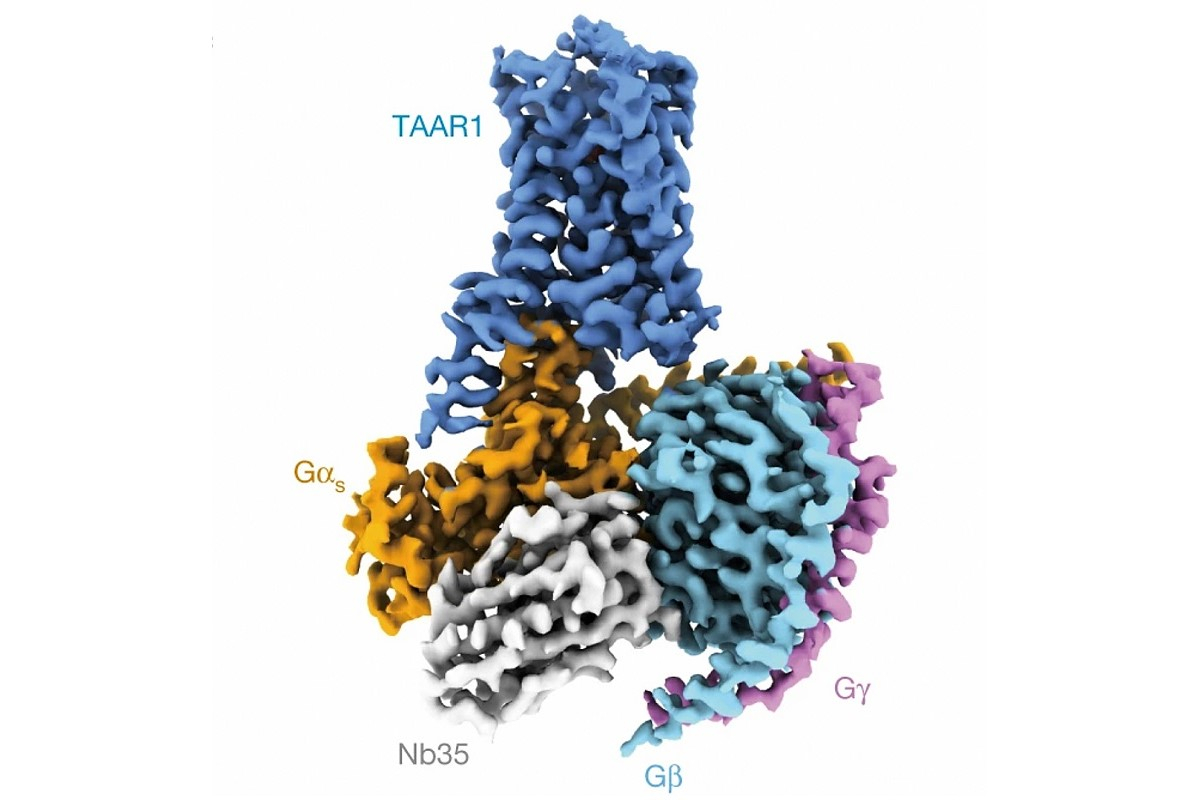
The Nobel Prize for the discovery and study of G-protein—coupled receptors was awarded back in 2012. These proteins are involved in a huge number of G protein-mediated signalling pathways in the body. Hence, they are often chosen as targets for pharmaceutical drugs. Nonetheless, about one fifth of this huge class remained understudied for a long time and seemed entirely uninteresting. Raul Gainetdinov, a winner of the 2023 Vyzov Award, Director of the Institute of Translational Biomedicine at St Petersburg University and Academic Supervisor of the Pirogov Clinic of High Medical Technologies at St Petersburg University, told N + 1 how it was discovered that these "uninteresting" receptors are activated by trace amines, act as "rot sensors" and they are, in fact, very promising drug targets for depression, schizophrenia, bipolar disorder and neurodegenerative diseases.
This article appeared in the Russian popular science online periodical N + 1 as part of the special project "This is for the future", supported by the Vyzov [Challenge] National Award in the field of future technologies. In 2023, the Vyzov Prize was given in four nominations: "Vision" — for creating a trapped-ion quantum processor; "Engineering Solution" — for the development of a technology to produce magnets based on high-temperature superconductors; "Breakthrough" — for advanced research in polariton-based computing platforms and for the development of an optical transistor; and "Scientist of the Year" — for discoveries in the area of dopamine system and trace amine-associated receptors, which enabled new approaches for pharmacological treatments of brain disorders. This year, a new "Discovery" category was created. It is an international nomination, an award for an important discovery that has influenced the development of science and technology.
Cured meat and sweat
The objects of your research have a mouthful of a name — trace amine-associated receptors. What are these receptors and how do they work?
I have always been involved in dopamine research, since my sixth year at the university. I studied at the 2nd Moscow State Medical University, and in my final year, to write my graduation project, I went to the Institute of Pharmacology of the Russian Academy of Medical Sciences in the Laboratory of Neurochemical Pharmacology headed by Kirill Rayevsky. His laboratory focused on the study of dopamine receptors and the development of new antipsychotic drugs. I began to study dopamine in 1988, and in 1992, I defended a PhD thesis. My mentor introduced me to the "dopamine club". I got to know personally all the leading researchers in this field across the globe: in America; Italy; Sweden; France; and other countries.
As a postdoc, I worked in Moscow for a while, and then, everything began to go to pieces. By 1996, my lab team had fallen apart and there was no money for research. So I decided to go to number one in the field of dopamine research in the world — Marc G Caron at Duke University (USA). I wrote him a letter, as we had already met at a conference, and he took me on. Marc G Caron was a postdoc associate of Robert Lefkowitz, who was awarded the Nobel Prize for his discovery of G protein-coupled receptors (GPCRs). I liked the atmosphere in the lab so much that I stayed to work there.
Then in 2001, new GPCR receptors were discovered. The thing is, when Robert and Marc discovered the first G protein-coupled receptor, they made a bold assumption that there would be many such receptors. Yet, they couldn’t have even imagined how many. The last number I saw was 831. Four per cent of the human genome are GPCRs.

What is a receptor? It recognises signals from the outside of a cell and transmits them into the cell, thus triggering biochemical reactions in the cell. Approximately 30-40 per cent of the drug targets in pharmacology are GPCRs: haloperidol; levodopa; morphine; cannabinoids; and antihistamines. A little later, it became clear that of the 800-plus known GPCRs, most are olfactory. And there were also about 150-200 so-called orphan receptors, whose ligands had not yet been identified. That is, it was not clear what these receptors could be "opened" with. In the orphan GPCR studies, it was discovered that they are activated by trace amines; and hence, the name "trace amine-associated receptors" (TAARs).
What are trace amines? What kind of substances are they?
Trace amines are amino acid metabolites, the products of decarboxylation of amino acids. They were discovered 40-50 years earlier than dopamine, serotonin, and noradrenaline. Interestingly, even though they were found earlier, trace amines remained a mystery — the last group of unexplored biogenic amines, because they are found in the body only in small, trace amounts. These are such compounds as: -phenylethylamine; tyramine; tryptamine; octopamine; and synephrine. To date, many more trace amines have been discovered.
Simply speaking, we are made up of 20 amino acids. If the acid part is removed from an amino acid, we get an amine. Hence, 20 amino acids means 20 trace amines. When we realised that each amino acid has its amine, we even compiled a "periodic table" of trace amines, which can be used to predict them. The table was published in one of our reviews.
Of the 20 trace amines, receptors have been found for 13-14 — in different animals. But even from class to class, the number of receptors varies greatly. For example, the zebrafish (Danio rerio) has 122 trace amine-associated receptors; humans have 6, and mice have 14. Since my research interest lies in human pharmacology, it is the six human TAARs that we have been studying.
How are these amines derived in the body? The first and most medicinal of the ways is by removing the acid part using endogenous decarboxylase. Each of us has these enzymes. Thus, amino acids are "cleaved" to form trace amines.
The second way is by removing the acid part exogenously, by bacteria that have decarboxylase activity. The fact is that trace amines are abundant in foods produced by bacterial fermentation — wine, cheese, cured meats, and beer. Take, for instance, dry-aged steaks. Trace amines are abundantly found in meat after it has been placed for two to three weeks in a dry-ageing chamber. Additionally, during fermentation, foods become infused with flavour because, as it turns out, trace amines in general are very tasty. Basically, both the olfactory receptors and the taste buds are GPCRs.
And the third way is by removing the acid part using our endogenous bacteria — the gut microbiota. Up to three kilograms of bacteria live in each of us, and they start "chopping" amino acids in the stomach. It is still unclear how this affects our bodies. Bacteria also actively inhabit our skin, where they carry out the same activity. Hence, each of us has a unique scent. Indeed, there are several mechanisms of body odour, but this is one of them.
Trace amines in medicine
No one had used trace amine-associated receptors as drug targets before you. How did you come up with this idea?
At the suggestion of my American supervisors, I took over the research of the new trace amine-associated receptors. My wife Tatiana Sotnikova and I worked in the USA until 2007. Then, we went to Italy, the country of trace amines: wine, cheese, seafood — these foods are high in trace amines. We are scientists; so, we decided that we should try on ourselves what we were studying, just as pharmacologists used to try what they synthesised. And we tried them every day.
By that time, the first knockout animals had already appeared, in which the gene for one of the trace amine-associated receptors — TAAR1, was inactivated. This means that the protein that is encoded by that gene is not synthesised.
I had a favourite animal model, the dopamine transporter knockout. The dopamine transporter (DAT) is the main target of cocaine and amphetamine. These psychostimulants inhibit the transport of dopamine by preventing the DAT from capturing dopamine back from the synaptic cleft, at the point of the contact between two neurons. When the DAT is "switched off", the amount of dopamine will increase five to six times and the animals become hyperactive. When the first agonist from among the trace amine-associated receptors — TAAR1 agonist — was found, we tested it on the DAT knockout animals, and they, as if by magic, calmed down.
The fact of the matter is that dopamine transporter knockouts are the best models for schizophrenia, as the main goal there is to suppress dopamine hyperactivity. All currently known antipsychotics block the D2 subtype of dopamine receptors. It appears that we began to develop an antipsychotic drug with a fundamentally new mode of action — through a different type of receptor. Why is it important to find a fundamentally new mode of drug action? The thing is, to get the FDA’s novel drug approval you have to be either "first in class", or "best in class". It is hard to make a medication that would treat schizophrenia more effectively than haloperidol. Indeed, it has a lot of side effects, but it works without fail. As for the "first in its class" substance, it has a completely different mode of action. That is the reason why we have such an interest in TAAR1 agonists.
And then, a research paper by Linda B Buck was published. Together with Richard Axel, they were awarded the Nobel Prize in Physiology or Medicine for their discoveries of odorant receptors and the organisation of the olfactory system. In that paper, Linda B Buck claimed that all TAARs in humans, except for TAAR1 that we were working on, are purely olfactory receptors. In other words, TAARs are expressed in the nasal olfactory epithelium and found in the olfactory receptor neurons, where an odour molecule binds to a receptor, which initiates a signal that travels to the olfactory bulb. Generally speaking, no one argued with that, but I am grateful to Linda B Buck for two other things. Firstly, she demonstrated that TAARs function as olfactory receptors that are responsible for innate odours. And secondly, she claimed that these receptors are not expressed in the brain.
Our innate aversion to some odours has a simple explanation: the smell of death. Dead body smell occurs when amino acids in the body are actively breaking down. The main components of the smell of death are cadaverine and putrescine, two products of decarboxylated amino acids lysine and ornithine. These compounds help herbivores to detect predators. A good friend of mine from Harvard University once published an interesting research paper. He went to a zoo and collected the urine of 400 different animals — both herbivores and carnivores — and the carnivores had high levels of -phenylethylamine in their urine. As it turned out, this organic compound is present only in predators, while herbivores can smell it. This is how a mouse, for instance, detects a cat. Why -phenylethylamine? Because it is a derivative of the essential amino acid phenylalanine, which is abundantly found in meat products.
So, the presence of this trace amine can be predicted based on diet?
Exactly. Herbivores sense that someone who has recently eaten meat is nearby; hence, they need to run and hide fast.
What is the role of trace amines and their receptors in pathologies?
This is a huge question. In any process that involves rotting tissue (which accounts for 80 per cent of medical cases), there will be trace amines. And inevitably, trace amine-associated receptors will be involved. A simple example: imagine that you have cut your finger. Bacteria get in there and begin ‘cleaving’ your amino acids. Thus, we get trace amines that will be targeted by leucocytes and monocytes that need to know where to go. A number of TAARs are expressed in white blood cells. That is, the trace amines help leucocyte chemotaxis and guide the immune cells to the right destination.
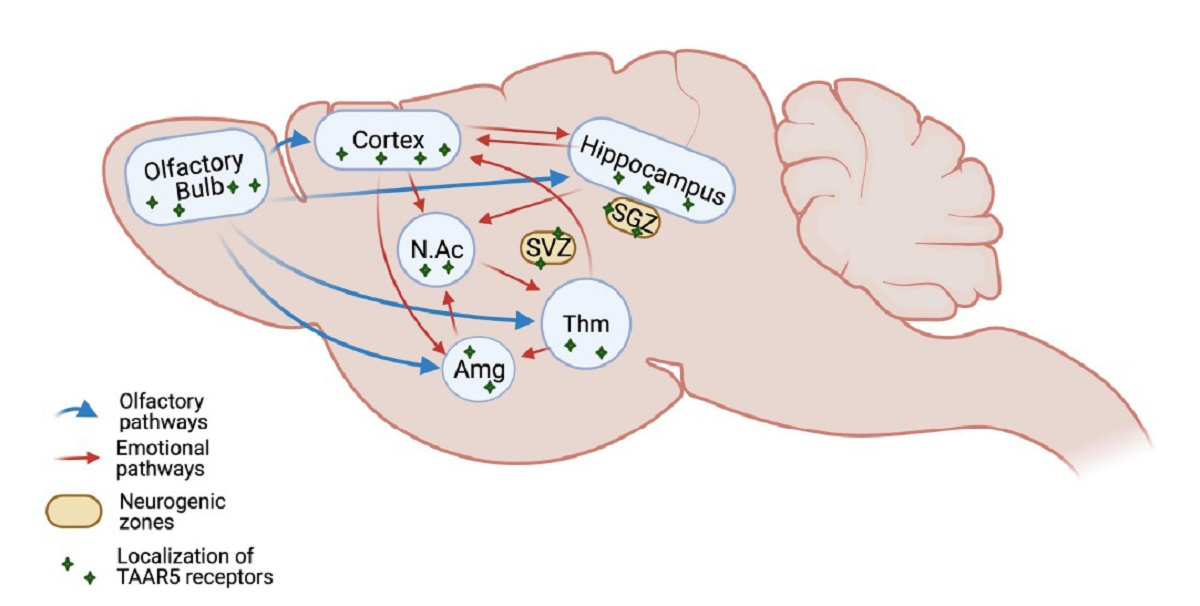
We made gene-targeted mice with a screenable marker to map the localisation of TAAR5 receptors. The marker staining showed regions where these receptors are expressed. Thus, we detected the receptors corresponding to this gene both in brain tissue and in the nasal olfactory epithelium. Importantly, we found these receptors in the limbic system, which is among the oldest structures of the brain, responsible for emotions. These structures receive signals from the olfactory system.
Then, the question arose: what do trace amine-associated receptors do in the brain? Could they become new drug targets? Because when we "switched off" TAAR5, the animals behaved as if they were on antidepressants. Thus, if we could find a blocker to these receptors, it could potentially become a new generation of anti-depression medications.
First, we found TAAR5 in the limbic structures and then around the ventricles of the brain, and specifically in the regions where adult neurogenesis occurs.
Now, imagine the following picture. These receptors are actually sensors of rot and they are localised where new neurons are produced. Or maybe they somehow sense the moment when it is necessary to switch on this system when neurons die; for example, after an ischaemic stroke.
We are trying to understand the role of TAARs specifically in the brain. For that, I created a unique collection of knockout animals.
Pine needles against rotten fish
It is a collection of mutant animals, isn’t it? What is unique about it?
We have animals with knockout of genes encoding all six human TAARs. There are five or six laboratories around the globe that have TAAR1 knockout animals, while we are the first to have a collection of knockouts for all six human TAARs. Our studies on knockouts for two types of TAARs revealed that these receptors are distributed slightly differently in the brain. Some are expressed more strongly in the amygdala, while others are expressed more in the hippocampus.
What is the main point of mutant animals? Once we have taken away a protein responsible for something, one particular TAAR, we see changes in animals’ behaviour or in the levels of dopamine or serotonin. Thus, we prove that this is a potential target. We can predict what would happen if a chemical agent blocked the receptor. Until such chemical agents, or ligands, are identified, gene-knockout animals are the only way to prove what the receptor, and any other protein, does in the body. This is the main advantage of gene knockout.
We know that antidepressants usually need to be taken at least for three weeks before the benefit starts to be felt. At the same time, as it has been found in animal models, neurogenesis doubles. The neurogenic theory of depression is based on this fact. We have gene-targeted animals that are genetically on antidepressants and with increased neurogenesis. One of my doctoral students is currently testing the effects of all TAARs knockouts and in five cases she has already found increased neurogenesis.
I really like the idea that trace amine receptor antagonists could be potential medications for the neurodegenerative disorders, such as Alzheimer’s and Parkinson’s disease. After all, one of the main hypotheses for these diseases is based on the fact that the rate of cell loss exceeds the rate of neurogenesis. These manifestations dominate the clinical picture of neurodegenerative disorders. For instance, Parkinson’s disease results from the death of dopamine neurons and is clinically manifested when 70 to 80 per cent of these neurons have died. We have tested this on our animals. Their neurogenesis turned out to be stronger. More dopaminergic neurons imply more dopamine. In other words, if someone is developing antagonists of these receptors, these would be potential anti-parkinsonian and anti-Alzheimer’s medications.
Trace amine-associated receptors respond to a number of compounds, including putrescine and cadaverine. These names are associated with decaying corpses. TAAR5 is activated primarily by trimethylamine. It is a metabolite of choline, an organic compound that we consume with food. Trimethylamine has a profoundly averse odour of rotten fish. It is synthesised in our body in pathological conditions — remember, for instance, the smell of rotten teeth. There are people who smell like that all the time because they have a mutation in the gene that produces the enzyme that breaks down trimethylamine.
Interestingly, TAAR5 is blocked by timberol, commercially used in the perfume industry as a pleasant coniferous fragrance. This was discovered by researchers from Germany. We double-checked their data to make sure that this was the case. It turns out that the TAAR5 receptors are activated by the smell of rot and are blocked by piney scents.
Timberol belongs to a class of compounds called terpenes; and there are about 30,000 known terpenes. These are good medicinal compounds in general. Whatever plant-based or folk remedy we take, terpenes are found everywhere. We tested some terpenes as an experiment only to find that they really work. Unfortunately, however, it has become difficult to order test systems from the USA: the price has tripled.
In other words, some diseases or just bad moods can be treated using certain therapeutic aromas? Do you mean that we have found scientific evidence for the effectiveness of aromatherapy?
It does seem that we are getting to the bottom of aromatherapy, its mechanisms of action. This is a tricky one. If you search for Wikipedia articles that contain the word "aromatherapy", you will see that it is categorised as alternative medicine. But if you go to PubMed and look at the number of papers with this keyword, you will find over 5,000 publications. Of these, probably about 500 are examining effects of aromatherapy on improving depressive moods.
Scientifically proven positive effects? Have they been confirmed in evidence-based studies?
Exactly right. In Japan, there is a therapy practice of Shinrin-yoku, or ‘forest therapy’ — a relaxing walk in a coniferous forest. It has been established that it helps with anxiety and depressive states. Moreover, in Japan, this is a time-honoured practice. Currently, they are conducting studies to provide scientific evidence for this practice. Not to mention the traditions of aromatherapy in China. There are about 300 research institutes that study medicinal plants there.
The triumph of intuition
In one of your interviews, you mentioned that few people were researching this topic since it was not considered promising. My question is why is that? Is it scientific to say "I believe" or "I don’t believe"? Is the concept of scientific intuition applicable here?
Scientific intuition plays a huge role. But in my case, it was not just a hunch. I immediately tested the first trace amine-associated receptor agonists that came along on gene knockout animal models and they had five times more dopamine. They were insanely fast — it would be impossible to calm them down. When I injected the compound in question, the mice calmed down. That was intuition coupled with experimental data.
My former boss Marc G Caron, once said at a Scientific Council meeting of the pharmaceutical company F Hoffmann-La Roche: "How many hundreds of medicines have been discovered through the study of dopamine, histamine, serotonin, noradrenaline, and adrenaline? Now, we have one last class of small amines — the trace amines. Why do you think there couldn’t be new drugs there as well? This is the last group of unexplored biogenic amines, and there are receptors for them. So why not?" Many people, however, were intimidated by the unknown that required a large financial investment.
It is quite interesting that everyone nowadays believes in the TAAR1 receptor. But I remember how, about a decade ago, I went to probably a dozen of companies in the West: in Germany, Denmark, Switzerland, and the United States. And wherever I went, I would tell them about these trace amines. And every time, they would say that I had interesting experimental data, but why these receptors cannot be found in the brain. Well, a new generation of equipment came along and everybody was able to see them. Now, they won’t ask me such stupid questions.
The same goes for other receptors. Linda B Buck reported that TAARs are expressed only in the nasal olfactory epithelium, but not in brain tissue — and the things stalled. She is a Nobel Prize winner after all. She knows what she is talking about, right? But she just homogenised the brain tissue for RNA extraction and found nothing. Yet, in certain groups of neurons, TAARs are indeed there!
Eventually, we were able to clearly see the localisation of these receptors in the limbic structures of the brain: the hippocampus, amygdala and others — where, in fact, our emotions are "buried". And we were the first to go in this direction.
About 100 research papers on the five other human TAAR receptors, apart from TAAR1, have been published so far. I have co-authored and published 50 of them worldwide. This is what I am grateful to Linda B Buck for — for stopping a lot of pharmacologists with her erroneous data. The olfactory receptors are not very interesting to pharmacologists; hence, they did not proceed any further.
There are still people in the West who are still sceptical about my conclusions. There are only three or four laboratories that share my opinion, including, by the way, F Hoffmann-La Roche.
We are actually talking about psychiatry. Despite the breakthroughs of the recent years in understanding the nature, diagnosis and treatment of mental disorders, many psychiatric hospitals in our country continue to provide very "harsh" therapy. There have been discussions regarding the introduction of targeted treatment in psychiatry for quite a while; yet, it still appears to be a long way to actual medical practice. What main challenges and possible solutions do you see along this path?
I think, we really need to raise awareness amongst the medical practitioners. I’ll give you a personal example. My father passed away about six or seven years ago. He had a peculiar combination of Parkinson’s and Alzheimer’s disease: both psychosis and parkinsonism at the same time. So, he was on antipsychotics. I persuaded him to come off aminazine, but continue to take haloperidol, which he was taking for the rest few years. If you gave him levodopa, a medication for parkinsonism, he went into psychosis because of the increase in dopamine levels. When you removed the levodopa, he would be just lying down. I suggested to the doctors that they should change his medications for newer, latest-generation drugs. I tried to give them some tips, since I have been a pharmacologist all my life. I told them that I was willing to find, buy, and send the medications to them. But they would not use them. They would say: we know that aminazine and haloperidol work, but we do not know these new drugs. We are afraid that something wrong may happen to your father. In fact, they never tried anything new.
The medications I suggested would have worked. Because these are antipsychotics without the side effect of neuroleptic parkinsonism. I know, in my father’s case, they would have worked.
In fact, they would have helped millions of such patients.
No doubt. I was a consultant for Sunovion, the US-Japanese pharmaceutical company that is currently developing a new drug to treat schizophrenia, a TAAR1 agonist. They were already conducting the last phase of the clinical trial, but unfortunately the trial failed in July 2023. Not because the medication was ineffective, but because the trial was carried out during the COVID-19 pandemic. It was extremely difficult to recruit patients with "real" schizophrenia at that time. Now, they will have to do it all over again, while their drug could have already been released in November 2023.
On the one hand, this is good news for us. We might be able to gain on the competition, because we are also developing such a medication. We are still at the early stages though. We need a few more years. It is, indeed, a long story.
Nevertheless, their preliminary data from the phase 2 clinical trial in schizophrenia was so good that the FDA granted that study a Breakthrough Therapy Designation status. This may potentially accelerate the drug’s release by two to three years. Why is it a breakthrough therapy? The data demonstrated its efficacy for all symptoms of schizophrenia and improvement of cognitive status. And most importantly, there were no side effects, as with haloperidol and similar drugs. In other words, this new medication will be perfect. I wrote about such medications in my 1992 thesis and I am nearing one only now — 32 years later.
Are you ready to predict what disease will be targeted first in future clinical trials in Russia, for which you are developing therapeutic agents?
Definitely depression and anxiety. I know well some people in the management of the company that is promoting Ulotaront. They say that if they had targeted depression instead of schizophrenia, the drug would have been released by now. They chose to target schizophrenia for purely economic reasons: antipsychotics are more expensive on the market than antidepressants. This drug, however, will work for both pathologies. And most importantly, it is completely safe.
Next on the list of targeted disorders would be alcoholism or any other addiction. There is already scientific evidence about such an effect. We are also working on post-traumatic stress disorder — this will be a fundamentally new drug for PTSD. Experimental data from pre-clinical animal studies are already available as well.
Then follow neurodegenerative diseases, that is, psychiatric drugs. In parallel, we will be observing other effects. For instance, it turned out that TAAR1 and other trace amine-associated receptors are very well expressed in the pancreas. This may play a positive role in the treatment of diabetes. This research topic is still understudied. The observations were made on patients with schizophrenia during clinical trials. Usually during treatment with antipsychotics, patients are gaining weight. In that case, however, they were losing weight, which implies their metabolic state was improving. These data are very interesting and encouraging.
The rat race
You had the opportunity to work closely in research teams in the USA and Europe before you returned to Russia. What is special about working there and here, in your opinion?
In terms of doing research, the USA was the easiest for me. But it is difficult for me to live there due to social isolation. You live your whole life as if under the COVID-19 restrictions; you don’t see anyone; you only go to work and home. At least it was like that where I lived. Duke University is a perfect place for work, but when during the day you see more deer than people, this starts to wear thin after a while.

Unfortunately, in recent years, there has been some decline in scientific research in the USA. It is not as perfect as it used to be, when I came to work there in the 1990s. Back then, people were coming to work at Duke University from across the globe: Germany; China; Japan; Italy; Sweden; and Switzerland. You couldn’t have made a career in research without being stewed in the US. Which I did: I lived there for 12 years, working in one of the best laboratories in the world, under a Nobel Prize laureate. In the USA, when you order something, in a week, it is on your desk, sometimes even in five days. Here, by contrast, I sometimes have to wait years for some orders to be executed.
Italy is messy and closer to us. Still, with a certain skill, you can live more or less well there. And life there is definitely more fun. The social life in Italy is much more interesting and there is a plenty of things to see. I went there mainly to be closer to Russia, because it is just too much hassle to fly across the ocean every time.
Here in Russia... Actually, I am still wondering how I managed to do it. I was able to create better conditions than I used to have in both Italy and the USA. Take, for instance, my collection of knockout animals. I wouldn’t be able to maintain it in Italy now, nor in the USA. When I worked in the USA, we had 46 lines of knockout model animals in our lab. Now, the cost of keeping laboratory colonies has tripled. There is no way we could afford to keep such a collection if we had to start now. There is rising inflation in science and research, while research grants have not increased much. Hence, it is incredibly difficult to secure a grant there now — they call it the rat race.
Here in Russia, as we all know, we have a million of our own challenges and daily struggles. No one says that everything is perfect here. A lot of things you need to plan in advance. You have to estimate roughly what experiments you will be doing in a year’s time, and stock up on essential items. Of course, it is not always possible to plan ahead, but at least I always find support at St Petersburg University. They even built a small vivarium for us. Indeed, it is a shared-access facility, but 90 per cent of the time it is at our disposal. I also receive great support from the Russian Science Foundation.
By the way, I like the Russian Science Foundation (RNF) very much. They implemented an American funding system — adapted to our circumstances, of course, but it is quite easy to write grant applications. Compared to the RNF, it is much more difficult now to prepare grant applications for American and European research funding agencies. There is so much bureaucracy there now that it is a nightmare! Whereas the RNF has a quite reasonable approach to this and does not impose restrictive requirements for really effective funding. There is, however, one drawback — excessive reporting. In the USA, you need to write a two- or three-page report on a grant at the end of the year. We have to write 70-80 pages.
Have you been affected by the sanctions?
Yes, they dramatically increased the delivery time and the price. Fortunately, we stocked up on all essentials and we have not felt any shortage yet. However, when you need something new — a complex device or a new test system — then, of course, you are facing trouble. But so far, we have been able to survive.
All my international friends are still my friends. We co-author papers and publish together. A few weeks ago, a paper was published that I co-authored with my Italians colleagues. Last year, we published a paper with Americans and two papers together with colleagues from Belgium, Italy and Germany.

